Introduction
Human oocyte cryopreservation (OC) has gained immense popularity in the last decade. Post removal of the experimental label of OC following expert consensus by the ASRM1, the technology gained momentum globally as an accepted clinical service resulting in a trend I describe as the ‘BIG FREEZE’. This concise review explores the trends in OC since 2010, based upon the transcontinental databases from the UK Human Fertilisation and Embryology Authority (HFEA), the USA Society for Assisted Reproduction (SART), and the Australia and New Zealand Assisted Reproduction Database (ANZARD).
Demographic trends
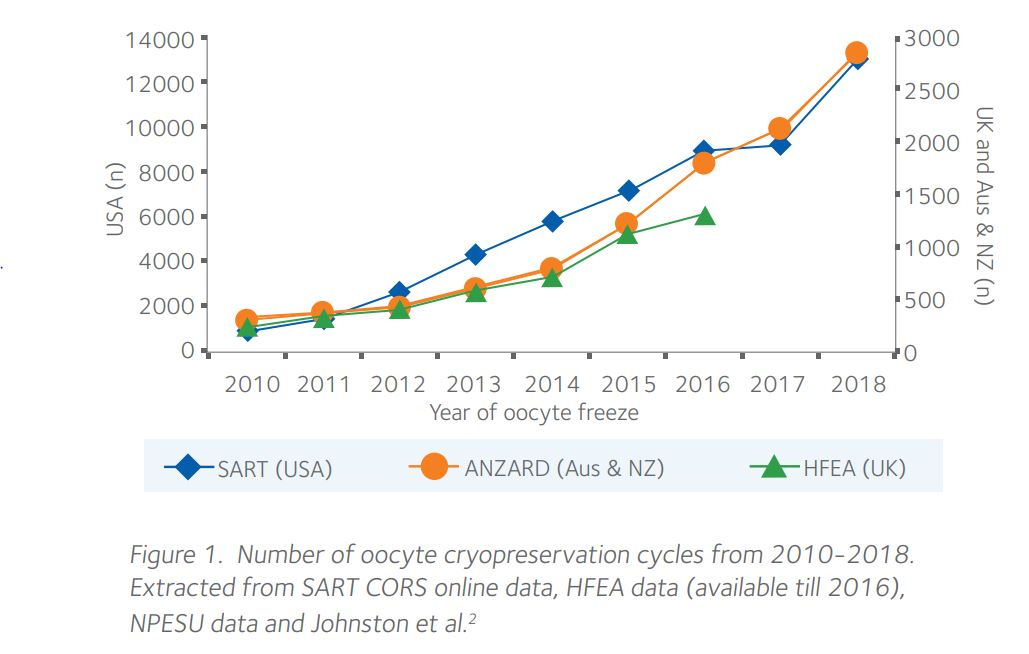
Rising trend in oocyte freezing cycles In the last decade, there has been a significant upswing in OC, as shown in Figure 1.
Trends seen in those coming forward to cryopreserve oocytes
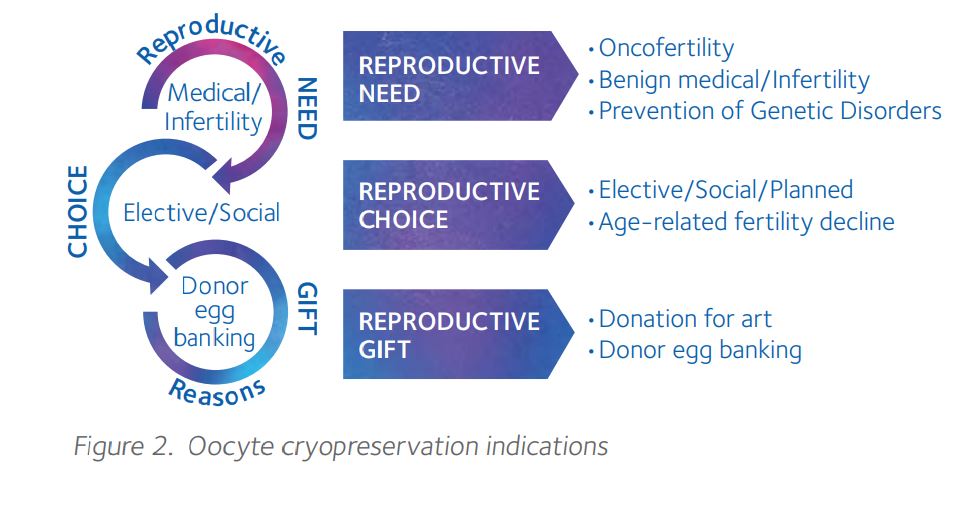
Indications for oocyte cryopreservation The indications for OC can be delineated based on three main motives, as shown in Figure 2.
Are more women coming forward to cryopreserve oocytes?
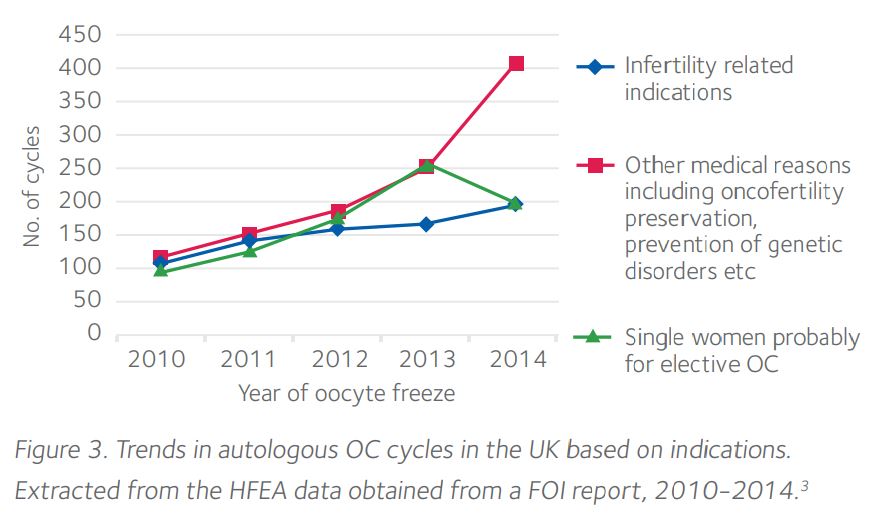
An exploratory review of HFEA data from a freedom of information (FOI) request3 in 2016 demonstrated that the number of single women freezing their oocytes had doubled in the UK over a five-year period (Figure 3) accounting for almost one-quarter of all oocyte freeze cycles in 2014. There has also been a significant 2.5-fold rise in OC for non-infertility-related medical reasons, reflecting improved awareness amongst nonfertility professionals, collaboration to initiate early referral and increased availability and accessibility of OC within the UK.
Are women cryopreserving oocytes at an earlier age?
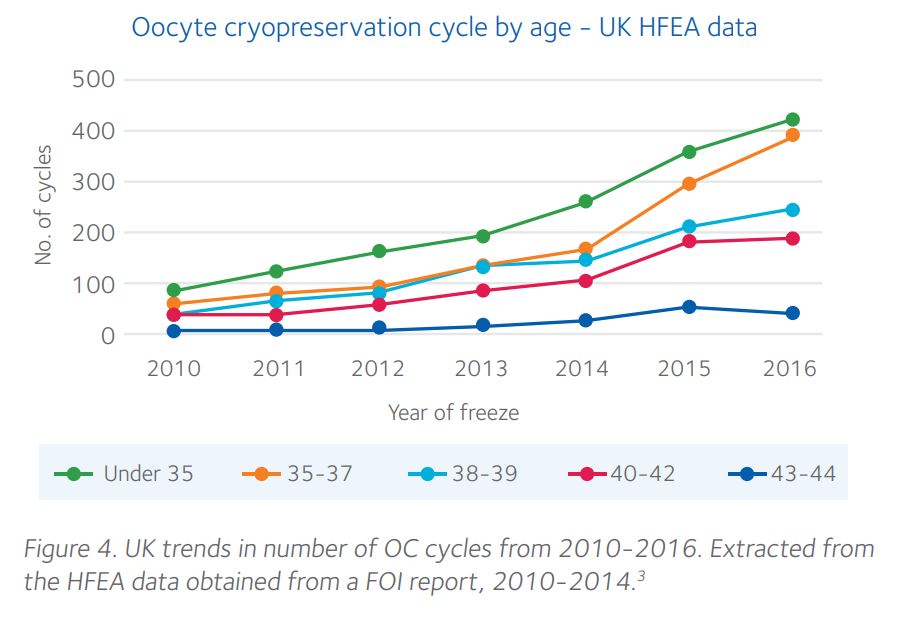
There is an upward trend in women seeking OC across all ages but the rise in women cryopreserving oocytes at <37 years has risen more markedly (Figure 4), though this data includes women donating oocytes.
Cryopreservation technique trends
The two universally employed cryopreservation techniques are slow freezing and rapid vitrification. With the higher efficiency noted with vitrification techniques, one can say that slow freezing has met a ‘slow death’ when it comes to the preferred cryopreservation method for oocytes in IVF clinics worldwide. Vitrification uses either an open or a closed carrier system. Studies have reported high survival rates with both open (85-90%) and closed (90-95%) techniques4,5 but data
on fertilization rates are conflicting with some reporting lower outcomes with the closed vitrification system.4-6
ART outcome trends
Our study7 looking at women aged <37 years undergoing oocyte thaw cycles in the UK over a period of 16 years, showed a lower live birth rate (LBR) of 22% for autologous frozen oocytes compared to 31% for donor cryopreserved oocytes (OR 0.63, 95% CI 0.46-0.86). When linked with age at freeze of <35 years, the LBR per thaw cycle in 2016 for women using their own oocytes remained consistently low at 15% in comparison to 32% in those using donor oocytes.8
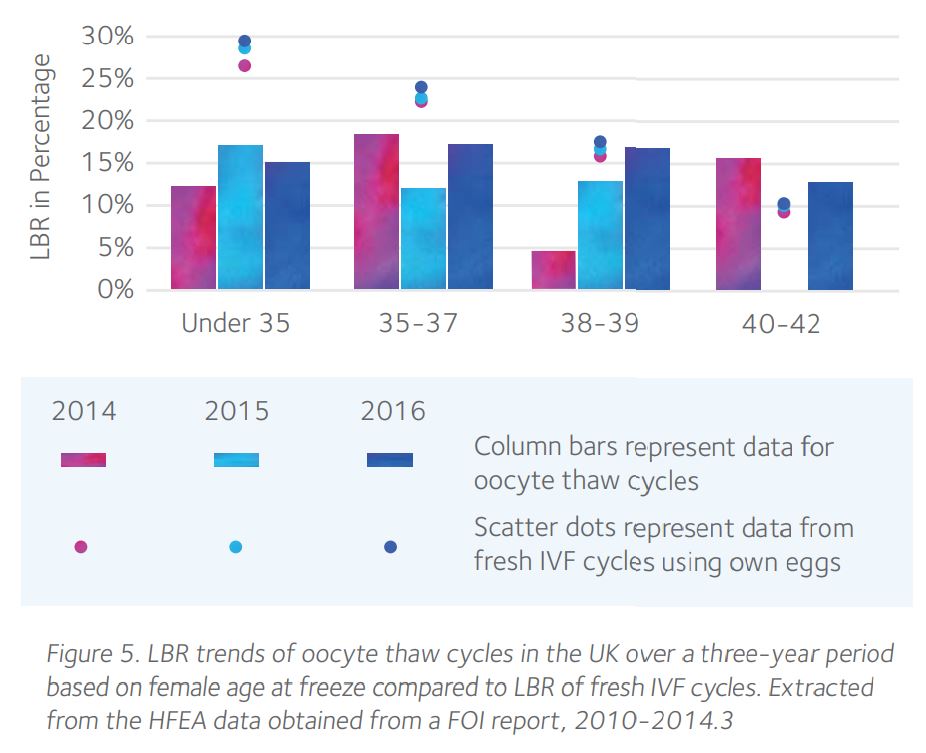
In comparison, a recently published HFEA report9 on the latest fertility trends suggests a LBR of 32% per embryo transferred for <35 years using fresh own oocytes in the UK. This is synonymous with frozen donor oocyte data but suggests plausibility of other confounding factors that may result in lower success with age-adjusted thaw cycles from frozen own oocytes as shown in Figure 5.
HFEA UK Trends in LBR for oocyte thaw cycles based on female age
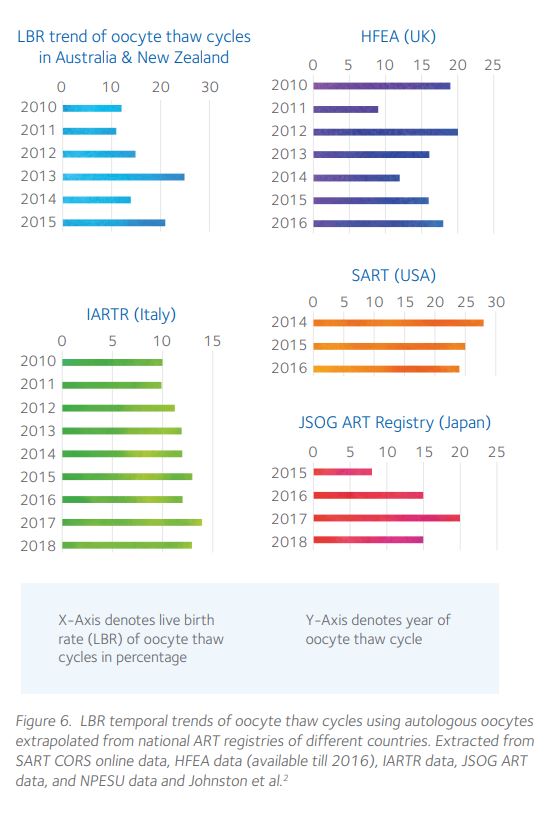
Transnational trends in LBR utilizing autologous oocyte thaw cycles demonstrate that the LBR has remained almost consistent in each country over the years (Figure 6).
Long term outcome trends
Our study7 based on HFEA data found a higher risk of low birth weight following frozen donor oocytes (14%) compared to autologous frozen oocytes (5%). Observational studies10, 11 to date have not reported a higher risk of congenital birth defects in offspring born following thawing of cryopreserved oocytes. Though data on long-term health outcomes are lacking, findings from a recently published study12 which reported comparable growth and health of children at two years of age (n=72) born from vitrification of donor oocytes vs fresh donor oocytes are reassuring.
Conclusions
The availability of national ART data registries gives us a golden opportunity to think BIG and analyze data collectively to obtain meaningful outcomes and statistical significance.
References
1. Practice Committees of ASRM and SART (2012). Fertil Steril 99:37-43.
2. Johnston M, Richings N, Leung A, et al, (2021). Hum Reprod 36:624-35.
3. HFEA Freedom of Information request. https://www.hfea.gov.uk/media/2252/f2016-00004-revised-data-for-eshre-oocyte-cryoprreservation-survey.xlsx
4. Pujol A, Zamora M, Obradors A, et al, (2019). Hum Reprod 34:989-97.
5. De Munck N, Santos-Ribeiro S, Stoop D, et al, (2016). Hum Reprod 31:377-84.
6. Paffoni A, Guarneri C, Ferrari S, et al, (2011). Reprod Biomed Online 22:292-8.
7. Mascarenhas M, Mehlawat H, Kirubakaran R, et al, (2021). Hum Reprod 36:1416–26.
8. HFEA Egg Freezing Trends Report, (2018). https://www.hfea.gov.uk/media/2680/final-egg-freezing-underlying-data-sheet-updated.xlsx
9. HFEA Fertility Treatment 2019: trends and figures, (2021). https://www.hfea.gov.uk/about-us/publications/research-and-data/fertility-treatment-2019-trendsand-figures/
10. Goldman K, Kramer Y, Hodes-Wertz B, et al, (2015). Fertil Steril 103:662-8.
11. Noyes N, Porcu E, Borini A, (2009). Reprod Biomed Online 18:769-76.
12. Van Reckem M, Blocke
 Meenakshi Choudhary MBBS MD PhD FRCOG
Meenakshi Choudhary MBBS MD PhD FRCOG
Dr Choudhary is a leading Clinician in Reproductive Medicine at the internationally renowned Newcastle Fertility Centre at Life and oversees the world first mitochondrial donor program.
Her key research interests cover reproductive ageing, recurrent pregnancy loss, improving ART outcomes, reproductive ethics and gamete donation.. She has numerous publications to her credit and is a global expert giving invited speaker talks at several international meetings. Her PhD research focussed on assessing factors that influence embryo donation and embryo development. She oversees the ethical and regulatory aspects of the research program at Newcastle Fertility Centre as the named Person Responsible for research for the Human Fertilisation Embryology Authority (HFEA). She is also affiliated to Newcastle University and Wellcome Trust Centre for Mitochondrial Research.
She leads the egg donor program and is also in charge of the new mitochondrial donor program for the world-first licensed treatment for mitochondrial replacement techniques. She is passionate about empowering women who volunteer to be donors and give a ‘gift of life’ to several women who suffer from infertility or deadly inheritable diseases. She believes in a ‘donor-centric’ approach keeping the best interests of the donors at heart without compromising the chance of a baby for the women needing these eggs.
She is a Trustee on the board of national UK Charity, Sperm, Egg, Embryo Donation (SEED) Trust. She sits on the National Institute for Health Research and Health Technology Assessment Prioritisation Committee advising on development of research topics related to mental health, women and child health. She also serves on the national executive committee of the British Society of Paediatric & Adolescent Gynaecology overseeing their website and patient information resources. She has also served on several national committees including the RCOG, association of Early Pregnancy Units and British Fertility Society.
Dr Choudhary published a number of publications in the field of Human Reproduction and have received several awards, the latest being the Asian Women of Achievement Award 2020 Finalist.

 My Clinic is in the United States
My Clinic is in the United States My Clinic is in Canada
My Clinic is in Canada