Preimplantation genetic testing for aneuploidies (PGT-A) is a genetic test designed to improve IVF success rates by providing information about embryos’ chromosomal status.
Embryos with the correct number of chromosomal material (called euploid) have a higher chance of leading to a successful pregnancy than those with the incorrect amount of chromosomal material (called aneuploid). Advances in PGT-A technology have introduced a third class of PGT-A results that lie somewhere in between. This additional class, deemed mosaic, contain a mix of normal and abnormal cells.
Embryos with euploid results convey one’s best shot at success, yet internal CooperSurgical data suggests that embryos with mosaic results account for, on average, 13% of all PGT-A-tested embryos*. That being the case, the most commonly asked question by patients when reviewing their PGT-A results is, “What would this mosaic result mean for a pregnancy or a baby?”
The answer is complicated. Embryos with mosaicism have always existed and been used in the IVF process, with or without knowing chromosomal make up. As more data is collected, it seems that, by and large, transfer of embryos with mosaic results does in fact lead to apparently healthy babies, albeit with reduced implantation and ongoing pregnancy rates depending both on the level of mosaicism (high vs. low) and the type of mosaicism (whole chromosome vs. segmental) when compared to embryos with euploid results.
However, there have been a limited number of case reports of babies born with abnormal chromosomal results consistent with the embryo’s original mosaic finding. Some of those resulting babies manifested with health complications as well (Kahraman 2020; Barad 2022; Schlade-Bartusiak 2022). Even so, it is unclear if this is above the typical background risk of birth defects (3-5%) for any pregnancy.
Listen to our podcast episodes on mosaicism
To help address this complicated topic, professional medical societies have made guidelines and recommendations to consider.
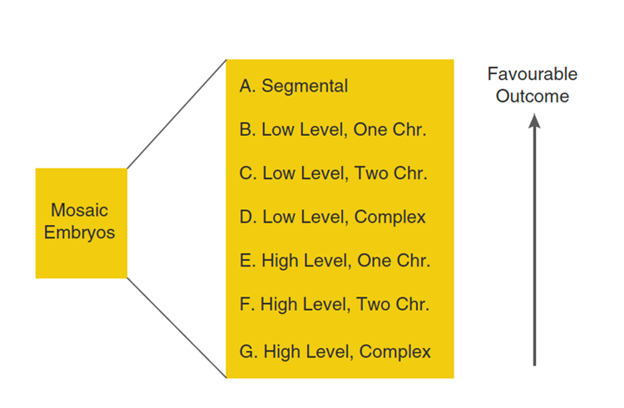
In 2021, the Preimplantation Genetic Diagnosis International Society (PGDIS) updated its position statement, recommending prioritizing embryos with mosaic results for transfer based on the following considerations: level of mosaicism, type of mosaicism, and/or the specific chromosome(s) involved. Prioritization should be primarily based on either the relative percentage of mosaicism, with low-level prioritized over high-level, or the type of mosaicism, with segmental prioritized over whole chromosome, with then the specific chromosome(s) involved being the last consideration, all depending on the embryo cohort. If levels of mosaicism among embryos are similar, transfer preference should be given based on morphology.
While the American Society for Reproductive Medicine (ASRM) released a committee opinion in 2020 that does not make specific recommendations regarding embryo prioritization, both this opinion and the PGDIS statement agree that any patient considering transfer of embryos with mosaic results should receive genetic counseling prior to transfer. If a pregnancy is then established, further prenatal genetic counseling and discussion of prenatal diagnostic testing options should be made available.
The images to the right, depict CooperSurgical’s mosaicism cut-offs, which can vary by testing lab.

Euploid
No or <20% abnormal cells
in the sample

Mosaic
20-80% abnormal cells
in the sample

Aneuploid
80-100% abnormal cells
in the sample
A Summary and Review of Recent Publications: Viotti et al. (May 2021) and Capalbo et al. (December 2021)
Viotti et al. recently published a study in Fertility and Sterility to help clinicians and patients make sense of mosaic results. Led by scientists out of the U.S., Taiwan, and Italy, this is the largest study to-date on the outcomes of transferring embryos with mosaic results, including 1,000 mosaic transfers compared to ~5,500 euploid transfers.
While outcomes indicate that embryos with mosaic results of any kind perform significantly more poorly than embryos with euploid results, the large sample size enabled further ranking of mosaic findings by likelihood for positive clinical outcomes, with segmental mosaicism of any level performing best, followed by low-level whole chromosome mosaicism, followed lastly by high-level whole chromosome mosaicism. Furthermore, this study found all live births from embryo transfers with mosaic results were reportedly healthy, and maternal age did not correlate with mosaic transfer outcome. Of the pregnancies that miscarried, the majority occurred within the first 8 weeks of gestation, leading the authors to speculate that embryos with mosaicism that implant will likely either result in an early loss or a healthy baby.
The following image outlines the recommendations of this study.
What other factors could be considered?
- What does your patient’s personal fertility journey look like?
- What has been the patient’s fertility journey thus far? Have they experienced multiple pregnancy losses, the loss of a child with disabilities, or no pregnancy to date?
- What is their current financial situation? Is another egg retrieval doable – physically, emotionally, and financially?
- What is the patient’s age? The risks of aneuploidy increase with age, especially the age of the egg contributor.
- What is the family’s comfort level with various risks – the risk of non-implantation, miscarriage, stillbirth, or the birth of a child with disabilities?
- What is the level of mosaicism?
- Depending on the genetic testing laboratory used, the level of mosaicism, i.e., what percentage of cells in the biopsy were found to be abnormal, can be reported. Based on Viotti et al, embryos with low-level mosaicism (those with 20-40% mosaic cells) are expected to implant more frequently and lead to less miscarriages than embryos with high-level mosaicism (those with 40-80% mosaic cells).
- Is the entire chromosome impacted or only a part of it?
- As demonstrated in the Viotti et al. paper, while embryos with partial chromosome gains or losses (segmental aneuploidy) have the same potential range of outcomes as whole chromosome mosaics, they overall result in lowest miscarriage and higher live birth rates than other types of mosaicism.
Clearly, the short answer to what things should be considered when deciding whether to transfer an embryo with mosaic results is: a lot. Talking with a genetic counselor can help patients work through many of these issues so that they understand their results and options.
It is often said that ‘it takes a village to raise a child’. In today’s ever-changing world of IVF, it can justifiably be said that it takes a village to even have a child – a village made up of reproductive endocrinologists, embryologists, genetic counselors, nurses, OBGYNs, etc. While many advances have been made since the first baby was born via IVF in the late 1970s, in many respects, we are still in this field’s infancy. Dedicated, caring professionals will continue to be the heart of a field that helps build families… while navigating the unexpected, tricky parts along the way. It will be fascinating to see what new technology and genetic tests we will develop as the field continues to evolve.
References
Barad DH, Albertini DF, Molinari E, Gleicher N. IVF outcomes of embryos with abnormal PGT-A biopsy previously refused transfer: a prospective cohort study. Hum Reprod. 2022;37(6):1194-1206. doi:10.1093/humrep/deac063
Capalbo A, Poli M, Rienzi L, et al. Mosaic human preimplantation embryos and their developmental potential in a prospective, non-selection clinical trial. Am J Hum Genet. 2021;108(12):2238-2247. doi:10.1016/j.ajhg.2021.11.002
Kahraman S, Cetinkaya M, Yuksel B, Yesil M, Pirkevi Cetinkaya C. The birth of a baby with mosaicism resulting from a known mosaic embryo transfer: a case report. Hum Reprod. 2020;35(3):727-733. doi:10.1093/humrep/dez309
Schlade-Bartusiak K, Strong E, Zhu O, Mackie J, Salema D, Volodarsky M, Roberts J, Steinraths M, Mosaic embryo transfer – first report of a live born with non-mosaic partial aneuploidy and uniparental disomy 15, F&S Reports (2022), doi: https://doi.org/10.1016/ j.xfre.2022.05.003.
Viotti M, Victor AR, Barnes FL, et al. Using outcome data from one thousand mosaic embryo transfers to formulate an embryo ranking system for clinical use. Fertil Steril. 2021;115(5):1212-1224. doi:10.1016/j.fertnstert.2020.11.041
Further Reading:
Subscribe Here to our scientific newsletter, ART Scientific. ART Scientific is a quarterly publication that explores current topics of interest in our industry. It is written by a community of experts in the field and has a science focus at its heart.
*Internal CooperSurgical data, CooperSurgical mosaic thresholds detailed in above article

 My Clinic is in the United States
My Clinic is in the United States My Clinic is in Canada
My Clinic is in Canada