
Quality was the focus at CooperSurgical’s ESHRE 2020 Symposium session ART Imitating Life: The Chicken or the Egg, with speakers exploring how to improve quality in the IVF lab and clinic.
Hosted by Steven Fleming, PhD, CooperSurgical’s Director of Embryology, the session commenced with a few words from CooperSurgical’s President David T Hansen. As stated in the United Nations Human Rights Charter, every person has the right to attempt to have a child. Mr Hansen stressed that we, in the ART field, work to make that right a reality for our patients, but we often fall short of that goal as many countries have a limited number of qualified embryologists, standardized protocols, access to high-quality training, and quality management systems that can push the field forward.
He urged all of the ART community to work together to make fertility treatment more accessible, improve our standards and our compliance to those standards, share data, and embrace emerging technologies that will take embryology to the next level. It was a thought-provoking introduction and offered good grounding for the following talks in the session.
The Key Role of Cryopreservation in IVF
Speaking next, Laura Rienzi, PhD, of Genera Centres for Reproductive Medicine, Italy, discussed the key role of cryopreservation in IVF. She called vitrification a “game-changer,” as it has improved the quality of IVF care in many ways.

She explained that vitrification can enhance the cumulative live birth rate by offering the opportunity for more than one pregnancy from a single IVF cycle. According to her research, this has significantly increased the rate of single embryo transfers and thereby reduced the rate of multiple pregnancies.1
Vitrification also enables cycle segmentation for patients who experience ovarian hyperstimulation syndrome (OHSS) and need to delay their embryo transfer. Additionally, it can give the lab more time to evaluate the embryo cohort by performing PGT.
Fertility preservation has been hugely impacted by vitrification, where women can now pause their biological clocks for medical or non-medical reasons, and this is great news. The gamete donation industry has also been positively impacted, as oocyte vitrification enables gamete donation across borders.1
While the benefits of vitrification are clear, embryologist skill is crucial to its success. Although survival rates post-vitrification and warming are very high from 2PNs to blastocysts, they vary significantly across operators.1 Vitrification is inherently inconsistent due to its manual nature.
Clearly, there is room for improvement. Standardizing vitrification procedures and protocols across the embryology field, as well as adopting automation where possible, may improve the precision of timings, volumes, and manipulations.
Watch the recorded session here to find out how vitrification can be applied to all stages of development with high efficiency:
Dr Rienzi went onto demonstrate how an IVF lab’s key performance indicators can be broken down into three categories: outcome KPIs, structural KPIs, and process KPIs. While outcome KPIs are usually the primary concern, she explained that IVF labs also need to consider various process risks, such as lab staff injuries, and structural considerations, such as the number of cryo tanks required relative to the number of cryo procedures performed.
On that note, Dr Rienzi addressed the elephant in the room. The adoption of widespread vitrification that has led to a huge number of cryogenic tanks requiring maintenance.
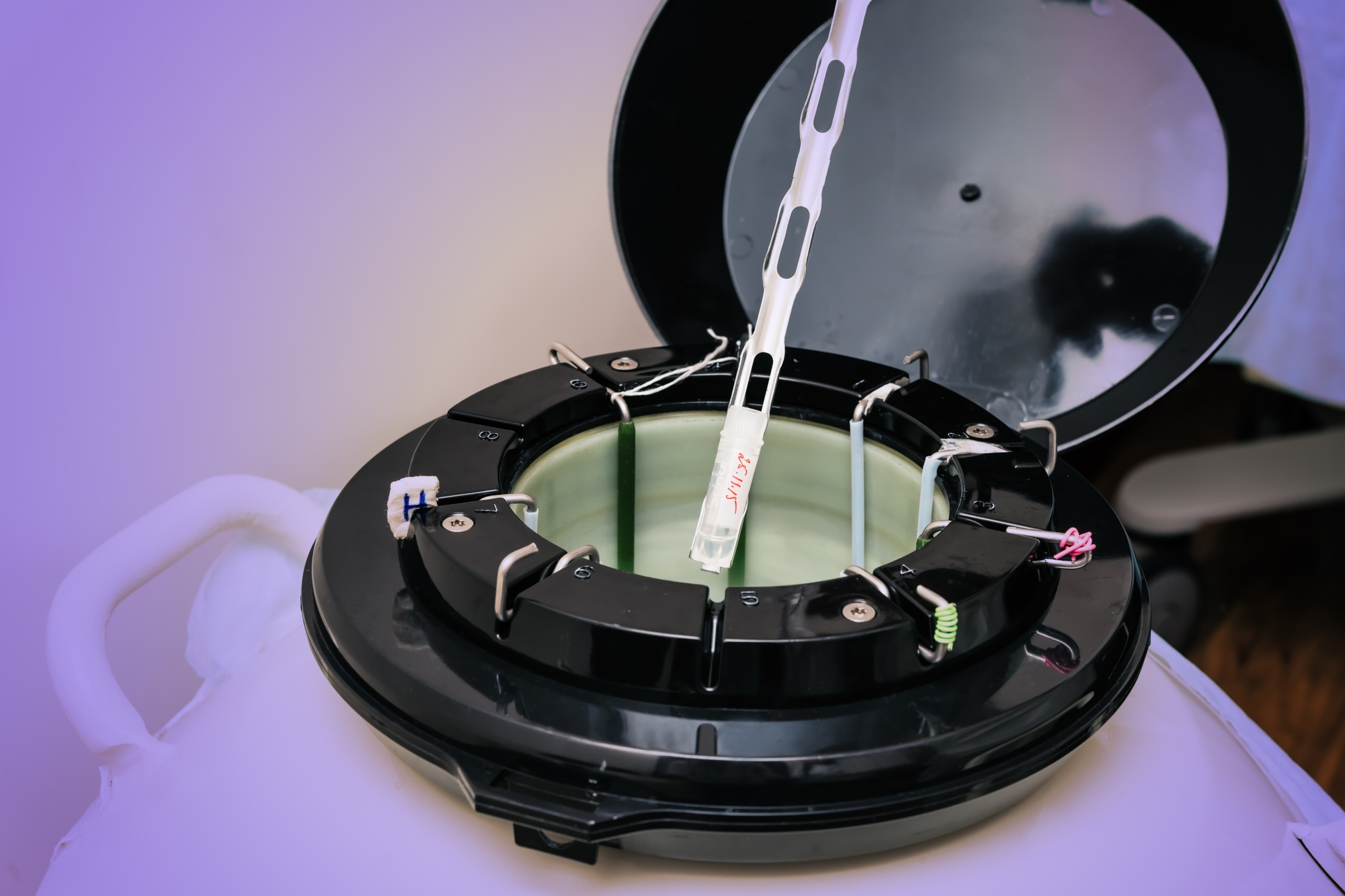
As the field has already seen, cryogenic risk management is essential on numerous levels. High-capacity tank systems may be ideal for long-term storage solutions given their several layers of protection against failure (such as alarms, digital systems, temperature sensors, etc). Efficient long-term record keeping and standardized labeling are also necessary to keep the system organized over time.
Vitrification is an essential procedure that has changed the structure of the IVF laboratory. Embryologists need to be able to cryopreserve at any time, at any stage. This requires a new level of flexibility. As Dr Rienzi demonstrated in her talk, in our increasingly technical world, embracing new advancements is important for today and tomorrow. Most importantly, optimized laboratory techniques result in increased safety for the IVF patient.
Quality in the IVF Clinic
The final speaker, Dr Willem Verpoest, Medical Director of the Centre for Reproductive Medicine at the University Ziekenhuis Brussels, Belgium, shifted gears by discussing quality in the IVF clinic. He began by posing a question: how do we define and measure quality in the IVF clinic?
He stressed that while quality in the lab relies on adherence to standardized procedures, quality in the IVF clinic is more holistic and less objective. Though many individuals may weigh in on a clinic’s quality, it is the patient who ultimately decides whether an IVF clinic meets quality standards.
Key performance indicators are one way to define and measure quality. According to Dr Verpoest, clinical KPIs can be broken down into cumulative live birth rates, hospital-wide functions, and center-specific considerations. Cumulative live birth rates, while nuanced in interpretation, can give information about the quality of an institution as a whole over a single individual or procedure. Administrative KPIs at the hospital level ensure that records are extensive, well-kept, and accessible.

Dr Verpoest went on to argue that center-specific performance indicators may be the most difficult to measure. While pregnancy rate per embryo transfer per operator is a standard measure, other metrics, such as pain score at retrieval, could also be used to gauge the patient’s perception of her experience.
But, if the patient determines the IVF clinic’s quality, how can the patient experience be enhanced and improve patient satisfaction? Dr Verpoest suggests clinics should invest in continuing education and training and allow senior staff to lead by example. Engaging in clinical research can improve long-term quality by pushing practitioners to consider novel methods.
He added that quality management systems are essential for managing processes, assessing risk, and proactively troubleshooting issues. Furthermore, the importance of cultivating a positive work culture among the clinic team cannot be underemphasized. Patients will be put at ease by friendly and harmonious interactions between staff.
Since patients are the true judges of clinic quality, Dr Verpoest suggested surveying them to gauge their perceptions. His clinic reportedly asks patients to complete questionnaires on multiple occasions throughout their treatment, from their first appointment to pregnancy testing and follow-up. Patients have the opportunity to give numerous opinions on their experience, from waiting room comfort and wait times to whether the physician was able to converse with the patient in their native language. This is a fantastic method for identifying areas to improve.
Collaboration is Key
In summary, all of the symposium speakers made it clear that clinic management, scientific organizations, certification and accreditation councils, and industry stakeholders need to collaborate to support clinics, education, and quality management. Patients are first and foremost in the assessment of a clinic’s quality; they can tell when a clinic is organized, educated, progressive, and cooperative. Our actions will let patients know they are safe, surrounded by a caring and knowledgeable team of experts.
Reference
1Rienzi L, Gracia, C, Maggiulli, R, LaBarbera AR, Kaser, DJ, Ubaldi FM, et al. Oocyte, embryo, and blastocyst cryopreservation in ART: systematic review and meta-analysis comparing slow-freezing versus vitrification to produce evidence for the development of global guidance. Hum Reprod Update, 2017; 23(2):139-155.
Author
Jenna Miller MS, CGC, is a board-certified and licensed genetic counselor. She holds a Bachelor of Science degree in Genetics and Biotechnology from Brigham Young University and a Master of Science degree in Human Genetics from Sarah Lawrence College. Jenna began her career at the biotech startup Recombine by providing genetic counseling services to patients and physicians. She then moved into clinical diagnostics, and eventually lead CooperGenomics’ carrier screening clinical diagnostics team. Jenna has been CooperSurgical’s clinical science liaison since 2017. In this role, she travels North America educating healthcare providers about genomics within the ART field.
Watch the Recorded Symposium
Bringing Quality to PGT
Read Jenna Miller’s review of our genomics ESHRE 2020 Symposium here.

 My Clinic is in the United States
My Clinic is in the United States My Clinic is in Canada
My Clinic is in Canada
