Jennifer Sloan talks about Genetic Counselling and what is covered during a pre-test consultation to facilitate informed patient consent.
Webinar Transcript: Genetic Counselling for PGT
In this webinar, Jennifer Sloan MSc CCRP talks to clinicians about genetic counseling. She speaks about the requirements for PGT-M and PGT-SR, outlines pre-test requirements and details what Cooper Genomics can consult for, to facilitate informed consent. Finally, she shares some feedback from patients and discusses the power of empathy.
Genetic counseling should not be confused with gene therapy! I do have to explain that to some couples. Most couples for PGT-M have already been through genetic counseling, clinically, in the NHS with our health care providers there. Others, perhaps, have had a diagnosis of a translocation at a fertility center and this is all new to them. Maybe they’ve not yet had an opportunity to speak to a clinician in the NHS (if they’re UK-based, of course).
What is PGT, PGT-A, PGT-SR and PGT-M?
At the very beginning we need to be clear on acronyms. PGT used to be called PGD (for ‘Diagnosis’); now the T stands for ‘Testing’. How I explain it to couples is I ask them to think of it PGT as a larger umbrella, with three terms beneath that:
– PGT-A (Aneuploidy) – basically the wrong number of chromosomes; any deviation from the 46 we see in the general population.
– PGT-SR (Structural Rearrangements): this includes your Reciprocal and Robertsonian translocations, inversions or insertions
– PGT-M (Monogenic) – for example, Cystic Fibrosis, Huntington’s Disease; well-known autosomal recessive and dominant inherited disorders.
What are the requirements for PGT-M?
This is often a question we get from clinics.
We are asking for clinics to send us any molecular reports that are available for either the patient or the partner as well as any other family members that have been diagnosed. If there are other reports that we have not received, we will feed that back that to our coordinator and the coordinator will ask the clinicians who are referring this couple.
We’ll also identify (depending on the inheritance pattern) who else in the family – either the patient or partner’s side – has an affected parent or child, or perhaps has had an affected pregnancy that perhaps we can get some of DNA from.
So, this is all part of the pre-test referral process for our genetic counsellor. Primarily it’s me assessing these but there’s also a senior genetic counselor from our US team that I’ve trained on UK specifics.
When there’s limited family members, we can do, sometimes based on the pathogenic variant, when we assess the molecular report, usually, if it’s a point mutation, that’s fine – we will speak with our laboratory and our scientists who are designing these PGT-M designs bespoke for each couple.
We also consider (obviously, uniquely here in the United Kingdom) whether there is HFEA permission for specific disorders. If not, clinics may apply for that before moving forward.
Some are quite unique scenarios that do warrant a clinical team discussion. We can have a larger team discussion with all our genetic counselors and our medical director as well.
PGT-SR Case Evaluation Process
In contrast to the PGT-M pre-test referral and inquiry process, for PGT-SR it’s a little bit different; we’re asking for a high-resolution g-banded karyotype. That’s generally what’s performed at either the NHS cytogenetic molecular labs or privately through TDL; I’ve seen quite a few those come out of London.
Our scientists will then do a calculation and personalize that for each unique patient or partner’s karyotype, and we’ll calculate the percentage of us identifying the unbalanced form of that translocation. That’s what we’re all interested in identifying so we can confidently report which embryos after next generation sequencing have either the balanced reciprocal translocation or Robertsonian (and I’ll get into that later, but basically we’re looking for right number of chromosomes – 46 – with our NGS).
Once that report’s written, we can notify the coordinator who will then notify the referring clinicians that we are able to accept this.
Pre-test PGT-M / PGT-SR Genetic Counseling
Pre-test PGT-M and PGT-SR genetic counseling sessions are quite different because there are different referrals for either monogenic disorders, Robertsonian or reciprocal translocations, so we counsel accordingly. Not everything that’s covered in a PGT-M session will be covered in a PGT-SR session and likewise.
Sometimes, either the male partner or the female patient has not yet had a referral to clinical genetics. Questions about translocation, such as ‘how did it happen’, ‘did I inherit it’, ‘did it happen by chance’ and ‘what are the repercussions for family planning and for my own medical health and management’ are all covered in a clinical genetic counseling session. So, when I speak to couples who have not had that session together I do compromise; I can’t spend two hours counseling everything so, I will summarise in a letter and I provide links to basic background information and an easy-to-follow video that’s narrated by our colleagues, genetic counselors in Ireland. We’ve had some feedback that that’s been quite helpful; I put the segregation pattern diagrams with either the Robertsonian or reciprocal translocation letters.
All our genetic counselors (including myself) always take family medical history from patient and partner. We begin that at the session, seeing if there’s anything else in the family history that could warrant a discussion or anything else that the couple are worried about.
We’ll do the brief overview on how our laboratory tests embryo cells and how we receive those from the referring clinicians at the fertility clinics. I provide a very brief overview – they’ve likely already had a consultation with one of your consultants at the fertility center – and just go over how our genetic testing fits into their whole cycle and care.
We aim to have a turnaround time of about two weeks (once we receive their embryo biopsies following their IVF fertility treatment) to have the analysis, interpretation and reporting done.
Pre-Test PGT-M Genetic Counseling
For PGT-M we include an explanation of Karyomapping; what it is and the accuracy of that. From the family history I’ve taken, I will identify and explain why it is that we’re asking for certain relatives to be involved in the test optimization or test creation process. I explain this in the very simplistic manner – I’m not making any assumptions that everyone’s had a PhD in genetics and is well versed with this. Certainly, if I aim quite low, in general, couples have spoken up when they do have a master’s degree or PhD, so they’ll let me know if I can adjust counseling according to their level of education and understanding the background reading
We have a new testing platform, PGTai. We’ve had that for quite a few months and now we’re coming up to release PGTai 2.0 and 2.0 plus. So, we do counsel the difference between them, depending on what’s ordered on the patient enrolment form, and we go over the accuracy.
I’ll also explain that, in addition to testing for the monogenic disorders or that specific translocation (the unbalanced form), we also include PGT-A, which looks at common aneuploidies in all the chromosomes. Sometimes I will explain how that happens when questioned and explain the term “non-disjunction”; how this usually occurs sporadically and how there is a correlation with maternal age as well.
Pre-Test PGT-M / PGT-SR Genetic Counseling
When clinicians order mosaicism, I will give a very brief overview. I will reassure couples that this may not be a part of their results at all; we see it in approximately 10 to 15% of results. When clinicians would like help from the fertility centers in explaining this to couples (if that is a part of their result) we’re more than happy to receive that post-test referral back to our genetic counselors here at Cooper Genomics. Whenever possible, whoever has completed the enrolment genetic counseling session (be that myself or one of the contracts counselors), will be the first choice for this next stage, for continuity of care. That’s quite nice, once you’ve already established that rapport with couples in a pre-test counseling session and enrolment session.
Here in the United Kingdom we’re all aware that the HFEA does not permit our laboratory from disclosing sex or gender of these embryos on the report. Obviously, there are exceptions for X linked disorders when that’s warranted. We will usually put ‘male affected’ and ‘female carriers’ or ‘X linked recessive’. And then, of course, X linked dominant is either male or female, so we would put ‘unaffected’ or ‘affected’ and we don’t disclose gender in that circumstance.
The accuracy of our testing is very high but it’s still not 100%, so we do recommend prenatal testing. If they have any further questions about CVS or Amnio (and the differences between those two; the accuracy, the risks involved etc) I do deflect all of those questions and encourage them to meet with a prenatal genetic counselor to discuss at length. If I start going there, I don’t get everything covered that I need from a laboratory pre-testing counseling session.
Very rarely, we’re unable to design a PGT-M optimisation bespoke for each couple. There are some circumstances where we’ve just asked for other cheek swab samples – perhaps we didn’t get DNA in sufficient amount or quality. Again, that’s very rare but we just don’t guarantee that every couple referred will have a bespoke test design offered and developed.
Once we have the DNA requested from everyone, we have a strict turnaround time for each of our scientists of approximately four weeks. When that’s finished, we will have our coordinator contact the referring clinician at the fertility centre to let them know that we’re ready to receive embryo biopsies for testing at any time.
In pre-test counseling, this is all part of our summary letter. It can be quite overwhelming so I will regularly check in with couples to check their understanding it all. I do also encourage questions throughout the session; it’s not meant to be a lecture; it is really meant to be a dialogue. I reinforce that, it’s very rare but, all of the embryos that we receive for testing may be affected (or aneuploid); likewise, some couples have found it hard to believe when we receive all the embryos and all of them are either unaffected and euploid.
We do provide, based on maternal age, the statistical probability for a PGT-A result – euploid versus aneuploid – and I do explain that that’s based on a large data set of internal results at Cooper Genomics from testing over hundreds of thousands of embryos.
I do say that the results will always be communicated by their referring clinician. I do provide a summary report for everyone’s records (the clinic’s, the patient’s and our own). I talk about the next steps in our consent form and sometimes, in special circumstances, there may be additional consent forms that are requested.
Estimated Euploid/Balanced Rates
PGT-SR also automatically includes PGT-A analysis. We do this concurrently because we use the same technology (so this is done by next generation sequencing after the embryo biopsies have been amplified in our laboratory upon receipt). I’ll speak about the estimated euploid rates and, again, when I’m saying ‘euploid’ and ‘aneuploid’ I will reiterate [the meaning of] these new terms that I’ve introduced to couples; ‘euploid’ = 46 chromosomes, aneuploid = any deviation from that (more or less). Sometimes that can even include partials – there are limitations from our current technology so that’s important to note as well.
For reciprocal translocations, our internal compiled data shows approximately ¼ or 25% are, on average, estimated to be euploid, Robertsonian approximately 30, inversions (and sometimes insertions) are a wee bit higher – 40 to 50%. Again, I reiterate that these are our best estimates when we speak, pre-test.
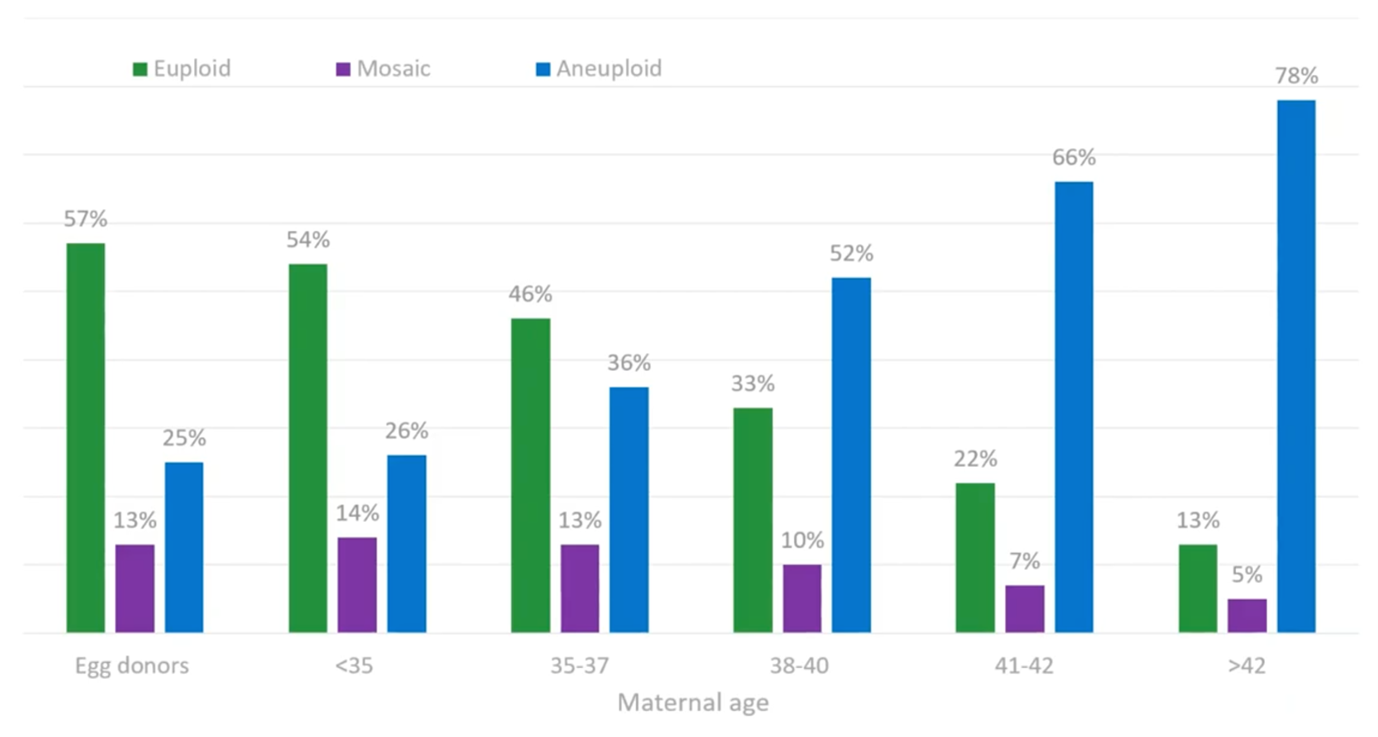
You may have seen this graph before. This is this a well-established trend that we’ve known for many, many years. The green bars are euploid (46 chromosomes), the purple are mosaic. Again, I mention that, on average, we see that about 10 to 15% [of the time, but] you can see that highlighted from the percentages in the purple bars. Conversely, the blue bars are aneuploid (the wrong number of chromosomes). An example I will highlight to couples to illustrate that is trisomy 21, also commonly known as Down’s syndrome.
A common question I get from couples is ‘do you test for everything?’ I do say that we can’t possibly do that from a genetic point of view; we’re focused on the specific gene, the very specific spelling mistake or genetic change or pathogenic variant for the disorder referred. If it’s a translocation, we’re looking for the unbalanced form of those chromosomes involved. And, more generally, with PGT-A, we’re looking at all the other chromosomes to see if there’s any aneuploid.
Counselling Benefits and Limitations
We do go over the accuracy for PGT-SR testing with next-generation sequencing. The primary take-home message from counseling here is that we are unable to distinguish, through next-generation sequencing, healthy embryos with the correct amount of chromosomes (46, euploid) that have a balanced reciprocal translocation or a balanced Robertsonian translocation versus the healthy embryos that do not have a translocation at all. They’re both going to appear as euploid (46 chromosomes) from our NGS results; we’re unable to distinguish the two. And I do emphasize ‘healthy’ because I do reiterate if it’s either the patient or the partner who has had the karyotype (who has this balanced reciprocal or Robertsonian translocation) I do remind them that their health is not directly impacting their medical management. Of course, the repercussions are for reproductive and family planning.
Very rarely, when Robertsonian translocations involve, let’s say, chromosome 14, I will always counsel about UPD – Uniparental Disomy testing. I’ll put a brief paragraph if I’ve counseled that and if that’s applicable, and answer their questions surrounding that. For NHS-funded patients it’s, unfortunately, part of the criteria for accepting the NHS funding, that that’s not permissible. But, for privately paid patients, if they do have a chromosome rearrangement (with a chromosome reported in the literature that’s to occur as uniparental disomy – for example, 14) that is counseled and offered.
So, it’s about really managing patients’ expectations. I will check in after I’ve given these numbers. I’ll ask…
- How are you feeling?
- Are you feeling overwhelmed?
- How are you responding to that number?
- Is that higher or lower than you expected?
- Did you have any previous expectations?
… just to elicit some feedback from couples, to get some sense of whether this is sinking in or if they’ve just zoned out after the first ten minutes!
It’s all part of effective communication. That’s the skill of genetic counsellors – not only taking complex genetic scenarios and terminology and explaining them very simplistically, but also compassionately and with empathy.
Effective Communication
A big part of our communication is our tone of voice, our cadence, how fast or slow we’re explaining something.
It’s important that we can hear if couples are distressed. Sometimes, when you’re taking family history, that can be very emotive for couples – I could hear someone crying. It’s really hard for them to tell me, a perfect stranger, 1.) over the phone, and 2.) very early in our phone consultation, about a parent who just passed away, or a pregnancy loss, or multiple pregnancy losses. So, all our genetic counselors are very, very sensitive to this and are trained. I’ve taken hundreds and hundreds of family histories over the years I’ve worked in prenatal both in public health care in private both in Canada and UK.
So, check in for support – particularly if there’s been a close loss or recurrent miscarriage. How are they coping as a couple?
Do they have close friends and family (and are they [friends and family] aware they’re [the couple] going through this PGT process? Sometimes, couples may not inform their friends or even their parents because they feel a pressure to keep everyone updated. Friends and family mean well – they want to they want to check in on you, they want to see how you’re doing – but after this counseling session they realize that couples are going through quite a lot. It can be very emotionally taxing as a couple (as we’re all very aware as clinicians) but also physically taxing for the women as well. So we acknowledge that and check which support systems do they have.
As I mentioned earlier, I will check in and invite some questions to try to elicit some response from couples – particularly if they haven’t asked much throughout the session. And I will check in and just ask, ‘has this been overwhelming?’ ‘Is this too much information?’ ‘We can always reconvene at another time depending on how you’re feeling.’
It’s all about establishing that rapport early in the phone call when taking the family history, using some empathic statements and normalization statements like ‘you’re not alone’, ‘I’ve spoken to many, many couples with a Robertsonian translocation’ or ‘…who has a child with cystic fibrosis’, or ‘who have had a family member with a sudden, unexpected death from a cardiac arrhythmia inherited cardiomyopathy’ etc). It’s not uncommon to feel and go ahead and identify those feelings.
You can tell, by the words the couples are choosing to use when they respond the questions I ask, what’s clear what’s not clear to them.
And I let them know that I am available (or whoever their genetic counselor is with Cooper Genomics). We’re not just a one-stop shop – not just pre-test; we are here if you have continued questions. I do my best to direct them back to the clinic whenever possible and I explain the reason we do this is because we want to ensure that anything coming from Cooper Genomics (either from our support team, our laboratory or our genetic counsellors) is all going through the clinicians so they are updated first and that both the couple and the clinics are receiving the same information at the same time. Once patients understand that, they appreciate that that’s the reason why we’ve set it up that way.
I say at the very beginning, this whole counseling session is to elicit better understanding. If they have any questions, they have an opportunity to [get] answers [to] those questions. It’s very much a dialogue, it’s meant to be a two-way conversation. Informed consent is a process. There’s no need to take notes; they’re welcome to if they want but I will provide a summary letter and the Cooper Genomics consent form as well. If they have any questions – specific things in the letter that are not understood – then I invite them for that feedback as well.
We’ll go over possible results from testing. There might be some clinic-specific information that’s communicated, for example, the possibility of a failed thaw when they have an embryo transfer set up and ready to go.
To adjust expectations, at the beginning of the phone call I do say we have about 45 to 60 minutes together. It may not take the entire time, it may take a wee bit longer if they have some questions. Some people are very visual learners so I will use diagrams and when they receive a summary letter, there’s links to videos that are narrated by our colleagues – genetic counselors in Ireland.
And I just ask them, ‘have you had any genetics knowledge – maybe in high school / sixth form? If there’s new concepts or terminology I’m introducing, I will reiterate that.
If English isn’t their first language, we do have interpreters. I’ve counseled people in Polish, Italian, Cantonese… several languages with the help of an interpreter and the same with our contract GCs. So, we have a team. It’s only me here in London but we do have a team of other contract GCs so we can accommodate it if couples are only available at evenings and weekends etc.
Patient Support and Feedback on GC Service
It’s been really heart-warming to hear some couples say, ‘thank you so much for your time’, ‘I really appreciate it’, ‘I understand’ and ‘thanks for taking the time to answer our questions’. One person said, ‘I can tell you really love your job’ and that was really nice to hear! I hope that is conveyed; that’s really what we’re here for. I said, ‘you’re not bothering me, you have my email (it’s in my letter). Please don’t hesitate to reach out if something’s not clear. If I don’t know the answer, I can direct you to the person who can give that to you.’
And on the subject of added support, for couples that are struggling with the recent loss of a child or family member, I will provide some local resources from my days counseling in the NHS. This is continuity of care; all of our GCs are aware of our new products and we can be effectively answering questions that are patient-specific or reference articles.
If there are any complex results, our laboratory director Leoni and I have spoken to couples directly, and sometimes couples and to clinics, or just clinics alone to help explain those results.
Impact / Power of Empathy
This video is a brilliant illustration about the difference between empathy and sympathy and the power and impact it has on people – particularly when they’re most vulnerable.
[It’s particularly useful when counseling those who are] going through a very difficult IVF treatment, together with genetic testing and the feelings and experiences surrounding that.
It’s narrated by a researcher in Texas – her name is Brené Brown. She’s had a couple of TED talks that have gone viral on the power of vulnerability and empathy, so I really, really encourage you to watch that. It’ll be helpful for yourselves, it’ll be helpful for your patients, and it’ll be helpful in your own lives, [helping you] connect with your family members and your friends. It may shock you if you can connect to the Bear or the Fox or the other character involved in that video. It’s nicely done.
About the Presenter: Jennifer Sloan MSc CCRP
Jennifer graduated from the University of Manchester’s MSc Genetic Counselling programme in the United Kingdom. Residing in London, Jennifer manages the UK contract genetic counselling team and PGT-M and PGT-SR referrals to our UK Cooper Genomics laboratory. She provides comprehensive genetic counselling for patient enrolment, results, and discussion of complex results with clinics and patients.
Read more about Jennifer Sloan MSc CCRP here.
Useful links
If you would like to explore any of the products / references mentioned in this article, please click on the links listed below:

 My Clinic is in the United States
My Clinic is in the United States My Clinic is in Canada
My Clinic is in Canada
